Safe Weight Loss Surgery in Mexico by VBariatric Welcome to our beautiful, brand-new Goodbye Obesity Center
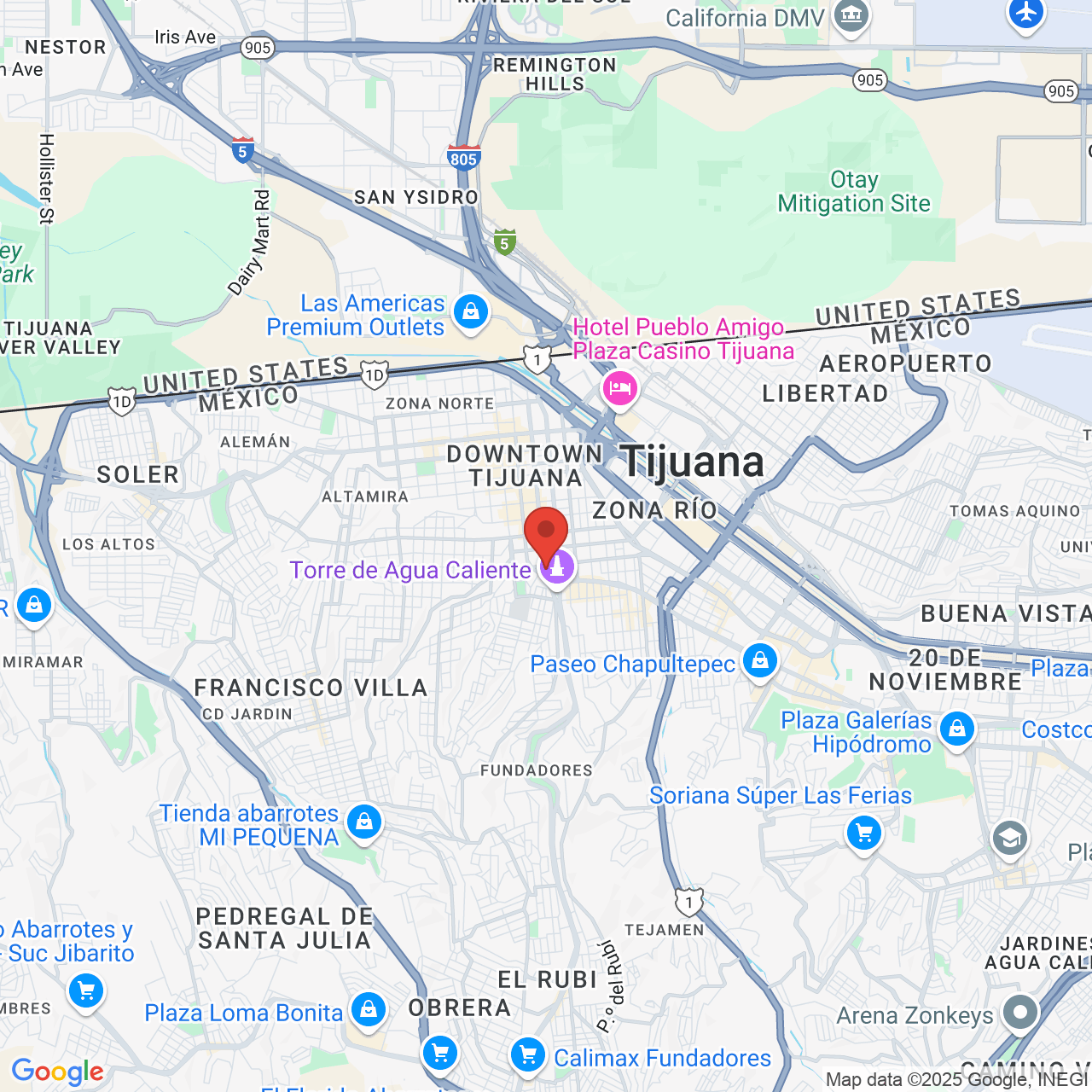
For over 25 years, Dr. Sergio Verboonen and VBariatric have worked together to help patients fight obesity and live long healthy lives through weight loss surgery. Dr. Verboonen is the founder of Goodbye Obesity Center, a state-of-the-art surgical facility located in the diverse, touristic city of Tijuana, Mexico. Because we are located just one mile from the US-MEX border, our VBariatric patient services team is able to offer high-quality medical care at a fraction of the cost of U.S. facilities.

VBariatric Personal Experience Process Convenience, Safety & Comfort
What Sets VBariatric Apart?
Local Team and In-House Services
VBariatric has a highly trained patient services team well-respected in the world of bariatrics, and we will be present when you arrive at the surgical center. Throughout your weight loss journey, we will provide unmatched support and guidance to help you in every way. Our pre-operative and post-operative care is carefully designed to help you maintain your weight loss for life. Also, when you call us, you won't talk to a call center thousands of miles away. You will be able to meet the person who coordinated your procedure when you join us in Mexico.
Fully Certified Bariatric Surgeons
Our board-certified surgeons have performed over 10,000 gastric sleeve and gastric bypass procedures, over 5,000 gastric band procedures, and over 4,000 other weight loss surgeries. All surgeries are performed by two fully certified bariatric surgeons. Because of their extensive experience, Dr. Verboonen and his team are known as one of the leading bariatric practices in Mexico.
State-of-the-Art Facility and Latest Technology
We own and operate our own surgery center with no intermediaries. This allows us to implement the highest quality standards for your security and comfort. We use the latest laparoscopic technology to perform bariatric surgery and advanced sterilization techniques.
Ready to Achieve Life-Changing Weight Loss? Schedule a Consultation with VBariatric
Are you tired of obesity affecting your health, mobility, and quality of life? With VBariatric, weight loss surgery is safe, affordable, and effective. Because Dr. Verboonen is one of the best bariatric surgeons in Mexico, men and women travel from all over Baja, the U.S. and Canada, and throughout the world to visit our weight loss center in Tijuana.
In addition to being a board-certified surgeon, Dr. Verboonen is a member of various prestigious organizations, including:
- International Federation for the Surgery of Obesity and Metabolic Disorders (IFSO)
- American Society for Metabolic and Bariatric Surgery (ASMBS)
- Mexican Council of General Surgery (CMCG)
- Mexico Board of Surgery for Obesity and Metabolic Disorders (CMCOEM)
To find out if surgery can help you achieve your weight loss goals, request a consultation online or call us: (619) 613-2560

"Thank you Dr. Sergio Verboonen for changing my life!!!"
Dr. Verboonen performed my gastric sleeve surgery one year ago. I flew from Texas alone and was naturally nervous but once I arrived in Tijuana, Mexico he and his staff took great care of me. He’s an amazing surgeon and I wouldn’t change a thing! I’ve presently lost 166 lbs and counting. Thank you Dr. Sergio Verboonen for changing my life!!!
View On GoogleI had my appointment with Dr Verboonen in June 12 after he explain and answer my questions I know I was in the right place .Had my surgery June 13 .The staff was very caring and helpful. My nurses Veronica and Luis did so much to help me with my recovery. I Highly recommend Dr Verboonen for anybody considering gastric sleve.
View On GoogleWhat We Offer
When you choose Dr. Verboonen as your surgeon, you will undergo bariatric surgery at our new, state-of-the-art surgical facility. Our facility is fully equipped to offer:
- Sanitation excellence and advanced sterilization techniques
- Unmatched presurgical and postsurgical care
- In-house patient services (VBariatric), lab work, x-rays, and fluoroscopy
- Preoperative and postoperative psychological and nutritional guidance
For your added comfort, each room has a TV, a bathroom, and air conditioning.
Meet Dr. Verboonen
Dr. Verboonen is a pioneer in the world of bariatric surgery. He has been performing weight loss procedures for over 28 years, and he is certified by multiple bariatric boards.
Our chief surgeon is a distinguished teacher, collaborator, and member of the most prestigious medical institutions in the country, and he has co-authored bariatric surgery textbooks that are used internationally. He is consistently recognized as one of the most distinguished bariatric surgeons in Mexico and throughout the world.
Dr. Verboonen has performed and mastered every bariatric procedure. In particular, he has devoted himself to perfecting the mini gastric bypass and sleeve gastrectomy procedures.
Featured Bariatric Procedures
Single Incision Gastric Sleeve
Single-incision laparoscopic surgery, or SILS, is one of the newest laparoscopic techniques. Unlike a traditional multi-port laparoscopic approach, this minimally invasive procedure is essentially scarless because the incision is hidden within the belly button. In general, the SILS technique takes about the same amount of time to complete as traditional laparoscopic bariatric surgeries, but patients may experience decreased pain and a shorter recovery period. The procedure is typically recommended for patients with a body mass index (BMI) between 30 to 39.
Gastric Sleeve
Also known as vertical sleeve gastrectomy, vertical gastroplasty, or sleeve gastroplasty, gastric sleeve surgery is another safe and highly successful option to help patients with morbid obesity. Most individuals with a BMI above 40 are good candidates for this weight loss procedure. Normally, gastric sleeve surgery takes between two and three hours to complete, but thanks to extensive training, our bariatric surgeons are often able to successfully complete the surgery in 50 to 60 minutes.
Mini Gastric Bypass
A mini gastric bypass is a restrictive and malabsorptive surgery that limits how much you can eat and changes the way that you process your food. Mini gastric bypass surgery is very similar to traditional gastric bypass surgery. However, instead of rerouting the digestive system at two locations, it requires only one reconnection. This surgery is suitable for most patients with a BMI of 35 to 60.
Revision Weight Loss Surgery
If you failed to see results after weight loss surgery, you may be a good candidate for a revision or conversion surgery at our Tijuana, Mexico, practice. The bariatric surgeons of VBariatric are experienced in many kinds of revisions, including converting a LAP-BAND® procedure into a sleeve gastrectomy.
Gastric Sleeve and Single Incision Gastric Sleeve Performed by Dr. Verboonen in Tijuana, Mexico
Take the First Step
With VBariatric in Tijuana, Mexico, life-changing weight loss is possible. Submit a patient eligibility form today to take the first step on your journey towards improved health and a new lease on life.
"Very Professional and Friendly."
I would absolutely go and get my surgery by Dr. Verboonen if I had to a million times! Staff was excellent. I had a great experience!!!
View On Google
Dr Verboonen and his team are amazing! I would recommend them to anyone. You will be treated with respect. They are very professional and friendly.
Our Weight Loss Services
Because we offer so many weight loss procedures, we can choose a surgery that fits your needs rather than one that fits our offerings. Dr. Verboonen currently performs:
- Gastric Sleeve Surgery
- Gastric Sleeve Cost
- Single Incision Gastric Sleeve
- Gastric Bypass Surgery
- Mini Gastric Bypass
- Bariatric Revision Surgery
- Revision Surgery from LAP-BAND® to Gastric Sleeve
- Revision Surgery from LAP-BAND to Mini Gastric Bypass
- Revision Surgery from LAP-BAND to Gastric Bypass
- Revision Surgery from Gastric Sleeve to Mini Gastric Bypass
- Revision Surgery from Gastric Sleeve to Gastric Bypass
- Duodenal Switch
See the Life-Changing Benefits of Bariatric Surgery in Mexico (real patient video)
"This place has outstanding service, everyone I came in contact with was so helpful and friendly. Starting with my phone call to setup my initial consult which they did at no cost to make sure I wasn't paying anything before I decided to start a program. Dr. Verboonen is certainly the right doctor for the his clinic after my detailed consultation they narrowed down to a few programs that made sense for my lifestyle. I think they truly do have an option for anyone trying to lose a lot of weight or just a few pounds! You can't go wrong here their prices are almost the same as others, but you get the added benefit of having the best weight loss surgeon in tijuana mexico." Laurie M.